Ohio Generally Prepared for COVID-19 Outbreak, Data Models Suggest
As the COVID-19 outbreak continues to spread across the country, statistical models produced by public health professionals show that, in comparison to other states, Ohio is well-prepared to weather the pandemic. While statewide testing rates continue to lag behind national averages, Ohio’s capacity of available hospital beds is projected to be sufficient to handle the peak of the outbreak.
As of Monday afternoon, 27,275 COVID-19 tests had been conducted across the state, with 1,933 positive results. By the same time, 475 Ohioans had been hospitalized with COVID-19, and 39 had died. Using population estimates from the Census Bureau, this reflects a per-capita rate of 233 tests conducted per every 100,000 residents.
In Lorain County specifically, currently-available data indicates that 82 cases have been confirmed, resulting in two deaths. Lorain County is one of three counties across the state that have declined to provide information regarding the specific zip codes where cases have been confirmed, citing privacy concerns while the overall number of confirmed cases remains low.
Across the United States, 964,865 tests have been conducted, or 292 tests per 100,000 people, meaning Ohio’s testing rates fall behind the national average. Nationally, 162,399 tests have come back positive.
Despite lower overall testing rates, the rate of positive tests in Ohio is much lower than the national average. Just over seven percent of Ohio tests have resulted in COVID-19 diagnoses; nationally, nearly 17 percent of total tests conducted have come back positive.
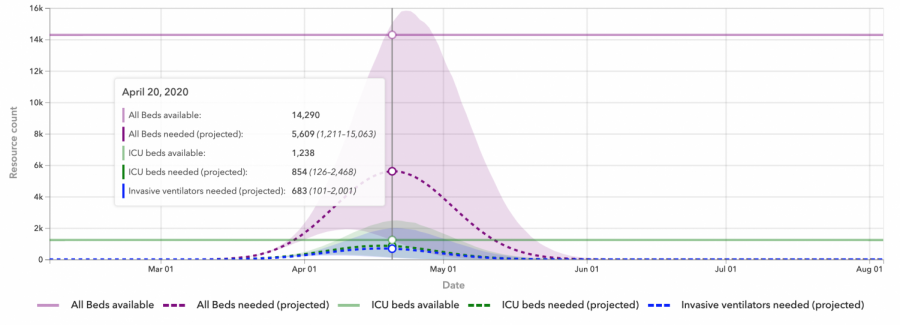
Further, available projections suggest that Ohio is better equipped than many states to handle the outbreak. Data collected by the Institute for Health Metrics and Evaluation at the University of Washington suggests that, even at the peak of the outbreak, Ohio medical facilities will have more than enough beds, including beds in Intensive Care Units, to accommodate the number of people who will need to be hospitalized.
The IHME model, which assumes “the continuation of strong social distancing measures and other protective measures,” projects that Ohio still has between two and three weeks before the statewide outbreak peaks. The currently-projected peak date is April 20. At the peak, the model estimates that roughly 5,600 of the 14,290 available hospital beds will be required to treat COVID-19 patients. Further, around 850 of the estimated 1,238 available ICU beds will be needed.
The available beds figures are calculated to account for beds that will be used for non-COVID-19 patients as well, based on average historical use. The number of available ICU beds is included in the calculation of total available beds.
In the projection’s worst-case scenario, patients around the state will require nearly 16,000 hospital beds, which would leave a shortfall of just over 1,500 available beds across the state. About 1,300 of that shortfall would be ICU beds.
Ohio is just one of nine states that is projected to have sufficient ICU capacity in order to address the outbreak, according to the IHME press release. By contrast, 11 states are projected to need at least a 50 percent increase in ICU capacity.
Similarly, death rates in Ohio are expected to be lower than national averages. According to the IHME projections, about 1,672 Ohioans will die from COVID-19, or about 14 people for every 100,000 residents. In the worst case scenario, the statewide rate of deaths per 100,000 residents climbs to 37.
Nationally, IHME estimates that in the United States, 83,967 people will die by August 4 as a result of the pandemic, or about 25 people for every 100,000. In the worst case scenario, 152,582 people die — about 46 people for every 100,000.
In states with more severe outbreaks like New York, the expected death toll is 81 deaths per 100,000 residents, and in the worst case scenario, the projected death rate rises to 108.
This IHME project is much more optimistic than reports released by other agencies, including one from the Centers for Disease Control and Prevention, which predicted a national death toll of 200,000 in its best case scenario. The worst case scenario was 1.7 million deaths.
“Any attempt to forecast the COVID-19 epidemic has many limitations,” the IHME researchers wrote in a paper published March 26. “Only one location has had a generalized epidemic and has currently brought new cases to 0 or near 0, namely Wuhan. Many other locations, including all other provinces in China, have so far successfully contained transmission, preventing a general outbreak. Modeling for US states based on one completed epidemic, at least for the first wave, and many incomplete epidemics is intrinsically challenging.”
Since the first case of COVID-19 in Ohio was confirmed March 9, Ohio Governor Mike DeWine has moved swiftly to address the potential for further community spread. Schools across the state were closed March 16, and a stay-at-home order was issued March 23.
DeWine has garnered national praise for his response.
“Ohio Gov. Mike DeWine’s coronavirus response has become a national guide to the crisis,” read a March 16 headline in The Washington Post.
Still, the governor has been critiqued recently for the state’s attempt to shut down abortion procedures, claiming they are “non-essential.” The American Civil Liberties Union contested the attempt in court and abortion procedures will, for now, continue to be performed during the pandemic.
More information about the statistical models discussed here can be found at https://covid19.healthdata.org/ and https://covidtracking.com/data/. Information specific to the outbreak in Lorain County can be found at https://www.loraincountyhealth.com/.